By Natasha Lukasiewich, DNP candidate, MSN, HHP, LNC, RN, CCRN-K, CFRN, CEN, EMS-RN and IPSA Mental Health Committee Member, Critical Response Team and Peer Support Unit Member for Washoe County Sheriff’s Office
How many times has one said this to themselves or have heard others say this, I want to help, but I do not know what to say? Sometimes, it is not about saying anything, and it is about the ministry of presence. Active listening and knowing your resources available are key.
When I was seven years old, my dad died by suicide. He died from severe depression, lack of support and not knowing what resources were available for him. From the coroners’ viewpoint, he died of carbon monoxide poisoning, but he also died of shame, guilt and a lack of knowing how to better his situation. Ultimately, he died of reasons unknown to those left behind and, more importantly, he is not here today.
This article presents a tool that allows one to check in with oneself and your colleagues. This tool needs no specifics, but a self-awareness based on color identification.
Health care professionals and first responders
What is happening in our industry of health care professionals and first responders? Think about the calls for service you have been involved with:
- Colleague overdoses on narcotics they have been diverting.
- Physician overdoses.
- Death by suicide on duty.
- Suicide by cop.
- Another staff member takes their own life by suicide.
These stories are not unique, and everyone could sit here all-day recollecting about how they have all lost some amazing souls in their time. Again, the same responses that occur over and over is often, I just don’t know what to say or do.
Shift workers all have shift changes, pre-brief, debriefs and so on. Why is so much of the health care and first responder industry focused on the hard skills and not the soft skills? Those who serve must be resilient and must improve all skills – hard and soft. Research shows that individuals who health care professionals and first responders serve are only receiving the care and service as good as the providers that are serving them.
Changes to implement today
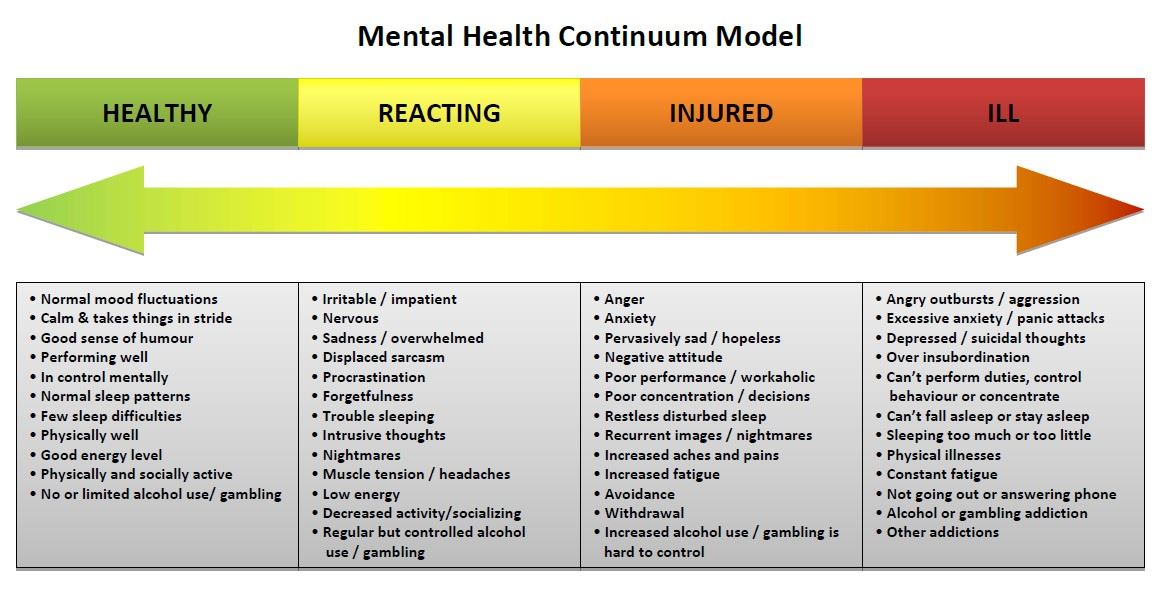
The challenge for each reader today is to implement what is called the mental health continuum model in your daily shift reports – adapted from the National Defense and the Canadian Armed Forces.
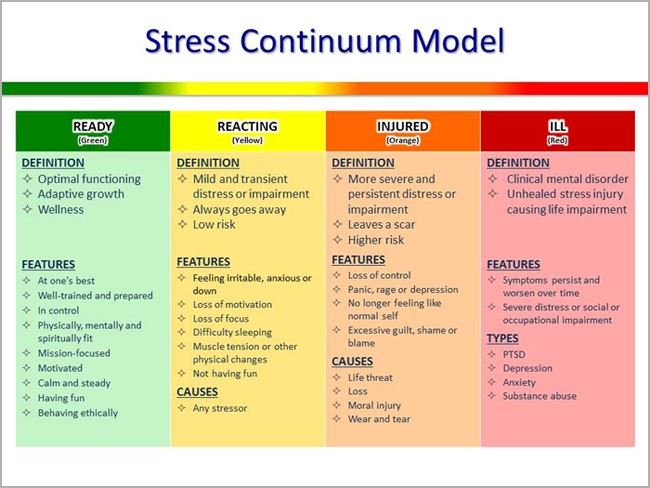
The Red Cross Crisis Response Teams worldwide also use what is called the Stress Continuum Model. This allows for the team leader to check in with those out in the field to see how they are coping with the horrific things they are being exposed to. See below.
Next steps
Now that the above tools have been shared and we have acknowledged that every health care professional and first responder must begin using them today, what are the next steps? Here’s an example about how to easily apply these tools in practice.
If you serve in an EMS agency, while doing crew change, the team lead can check with the crews and simply ask, “What color level is everyone today?” Without even knowing the details, a crew lead can assess mental readiness to the start of the shift. They have just triaged their team’s mental readiness.
The team lead can also check in after a bad incident – such as after a horrific pediatric call. Teams may have started off their shift in green or yellow, but after the call some of them are likely to be orange or red. If there is a significant shift in color after a bad call or shift, then there needs to be a tactical response to ensure the appropriate resources are dispatched or in contact with the health care professionals or first responders that need it, preferably, sooner than later.
Perhaps if my dad, or my colleagues had some sort of communication tool, they too could have been saved or at least been shown they were not alone.
The health care and public safety industries need to take mental health readiness seriously and regularly assess their personnel. These industries need to stop being reactive and be proactive with mental health readiness.
Try it, challenge yourself, challenge your organization. What color are your today?
About the Author
Natasha Lukasiewich started her journey in Health Care back in 2001, when she graduated from Grant MacEwan University, in Edmonton, Alberta, Canada with a diploma in Holistic Health. She later graduated from the same university, and completed her Nursing Diploma, venturing into Emergency Medicine. In 2006, she was recruited central coast California, to continue her ER nurse journey, later becoming a flight nurse for Calstar. She then continued her flight nursing career in Lake Tahoe/Reno, NV areas with Care Flight. In 2017, Lukasiewich completed her MSN and is currently completing her DNP (Doctorate in Nursing Practice). Her focus is primarily peer advocacy and raising mental health wellness in health care and first responders. She has been an invited speaker for many webinars, symposiums and national conferences on the effects of PTSD, depression and suicide for health care and first responders. For the last six years, she has served as a Volunteer Auxiliary Deputy Sheriff on the Washoe County search and rescue team, and also serves on their Critical Response Team and Peer Support Unit. You can connect with Natasha on LinkedIn or connect via her business website at www.legalnurse.solutions. Feel free to email her at natasha@legalnurse.solutions.
Related Content
IPSA Infogaphics: Depression, Suicide and PTS
Webinar Recording: Mental Readiness: Stigma Reduction & Resiliency Program
Webinar Recording: Fighting addiction in EMS/Healthcare
Webinar Recording: Heroes are Human Too: PTSD, Depression & Suicide